News

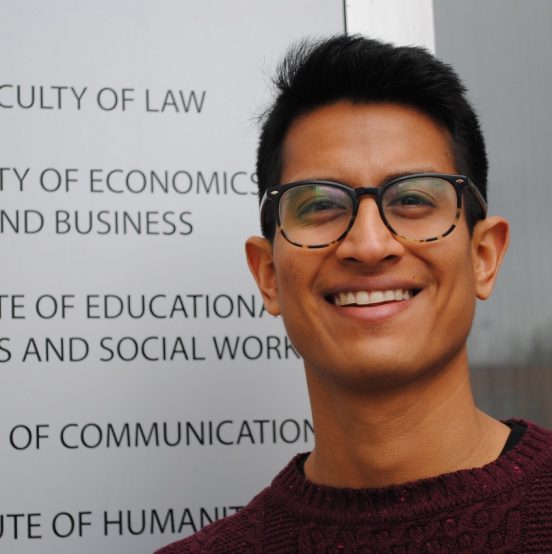
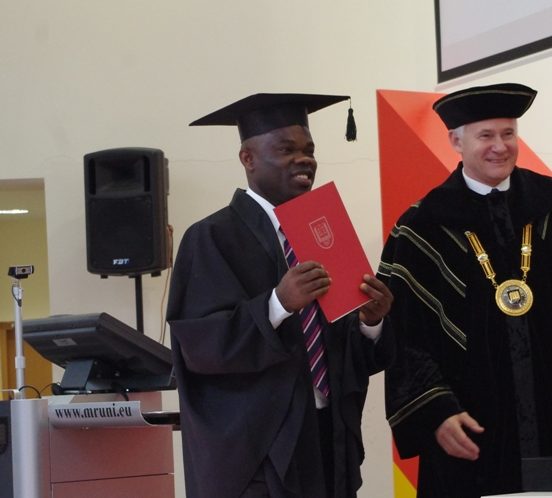
Feb. 5th, 2021, MRU PhD student Tomas Vedlūga (Leadership and Strategic Management Institute) successfully defended his doctoral dissertation, "Electronic Health System Evaluation Models." Research supervisor - Prof. Dr. Birutė Mikulskienė.
Defence Committee:
Chairman – Prof. Dr. Vainius Smalskys (Mykolas Romeris University)
Members:
Prof. dr. Danguolė Jankauskienė (Mykolas Romeris University);
Prof. Dr. Rimantas Stašys (Klaipėda University);
Assoc. Prof. Dr. Ermo Täks (Tallinn University of Technology, Estonia);
Prof. Dr. Jan Žukovskis (Vytautas Magnus University).
The goal of the dissertation is to better understand effective and ineffective e-health system determinants, identify user expectations and problematic aspects in the development and implementation of the e-Health system.
RESULTS OF THE ELECTRONIC HEALTH SYSTEM RESEARCH
In summary,
In summary, the biggest failures of the eHealth system are its coordination, lack of proper processes and procedures, actions of the healthcare institution administration, IS support, hardware and so ware problems, and user behavior. Ministry of Health of the republic of Lithuania (hereina er – MH) did not ensure centralized coordination of e-health system projects, which resulted in the risks of project implementation not being managed and deviations from the planned deadlines. Separate funding was also provided for e-health system projects implementing similar solutions, which did not save money and did not reduce the risk of integration between the IS under develop- ment. One-sided, formal MH communication with project promoters and partners was found to be non-feedback. e MH did not pay due attention to the performance of the SPS IS, according to the provision that the health facilities are responsible for the results of the projects, and the MH itself is only responsible for the national ESPBI IS. MH did not ensure su cient user involvement, e.g. the need for the participation of State Health Insurance Funds in the development of an e-health system, which does not include schools, kindergartens, employers, etc., remained underestimated. e developed functions of the e-health system do not meet and do not meet the needs of a speci c health facilities. E-forms are complex, inconvenient for unskilled users, there are excess lling elds, the logic of lling e-forms is unclear. ere are no clear procedures for lling in e-documents, only the procedure for lling in e-prescriptions is speci ed in more detail. Smaller health facilities do not have permanent IT sta and the knowledge and skills of their existing sta are insu cient to train users. e inef- ciency of the management of the health facilities is also visible: the implementation of the health facilitie’s internal procedures and plans for the use of the IS is not ensured, in some health facilities the IS commissioning acts are signed only formally, but the created IS is not used in full. Some health facilities do not pay enough attention to project partners, are not interested in their problem areas, provide only minimal assis- tance. ere are a number of technical errors: integrations do not work in full, e.g. the Sveidros IS number of the reimbursed medicine is transferred manually, incorrectly shows the data of doctors’ quali cations, positions, departments, roles or the data of the family doctor is not updated (2017). ere is a lack of computerized workstations (computers, scanners, printers). Doctors have electronic signatures, but not everyone has the technical ability to sign: there are no scanners (2017). Finally, the attitude of the users themselves is not appropriate: the habit of physicians to use a previous MS or to record health history data on a paper patient health record card. Doctors feel afraid to immediately con rm the written anamnesis and sign the e-signature, worried that the e-document will not be saved or disappear. And most importantly, doctors do not understand and do not get the real bene ts that an e-health system can provide. How- ever, there are also positive developments in the e-health system: e-prescriptions are being issued more and more o en, almost all health facilities can be registered online, health facilities share research results, and patients have access to their health infor- mation. However, societal progress is faster than improving the e-Health system itself, e.g. mobile devices and mobile apps have made a breakthrough, are user-friendly and o en represent computers. At present, no mobile e-health system application has been developed that would allow patients to conveniently access e-health system records or take advantage of pre-registration on a mobile device. Healthcare professionals do not have the ability to process patient personal data or issue e-prescriptions on a mo- bile device. All of these changes affect the culture of health facilities: thinking, values, norms, behavior, and communication change little by little.